A Panda Campaign
The WHO Paradox
Corporate Dominance in global public health
Campaign Update
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
Global public health, previously focused on community-based participation and poverty-reduction, has moved over the past 2 decades to a centralized, corporatized paradigm promoting pharmaceutical-based solutions in an increasingly vertical system. This is being justified by a health catastrophe /pandemic preparedness campaign that uses fear and targeted funding to overcome its obvious fallacies.
PANDA believes that this must be addressed urgently and systematically to expose the falsehoods on which the approach is based. This will undermine the drivers of the centralization of wealth and power that this corporate takeover of global health is supporting, which must then lead to fundamental reform of public health funding, conflict of interest management, and decentralization of health policy.
Get the Background
The Pandemic
Preparedness Fallacy
A myth of growing pandemic risk has been promulgated over the past two decades, coincident with growing corporate / private funding and influence over the World Health Organization (WHO) and the global health area in general. This is being used to leverage unprecedented funds directed to a mainly Western-centered industry growing around ‘pandemic preparedness’. It is, essentially, a massive shift in wealth through ‘aid’ funding, from Western taxpayers to Pharma-related entities, at the expense of these taxpayers, and the populations of low-income countries to whom aid was previously, at least nominally, directed. Large corporate structures, especially the World Economic Forum (WEF), have been very prominent, perhaps instrumental in this.

Pandemic Preparedness: The Facts
Pandemics are not increasing.
However, viruses are detected more readily through surveillance (eg. the use of PCR to increase reported Covid-19 cases). The WHO records only 4 pandemics in the 120 years prior to Covid-19.
Pandemics are not getting worse.
None since 1918-19 (including Covid-19) have had a major impact on overall mortality (and especially not among young and middle-aged people). It is generally considered that most deaths in 1918-19 were caused by secondary infections due to a lack of antibiotics then. Advancements in medical care including the availability of a wide range of therapeutics have substantially reduced the risk of mortality.
Human contact with wildlife is not increasing.
This is an obvious fallacy but widely used to justify greater funding for pandemic preparedness. Humans have lived closely with domesticated animals for thousands of years, and traded and trapped in the wilderness. There is now far less wilderness, far less wildlife, and human contact with wild animals is concentrated in fewer areas.
Large historic outbreaks were probably bacterial.
Bubonic plague is a bacterial disease (Yersinia pestis – the cause of the Black Death and Jusitinan plagues among other outbreaks). Cholera was a major cause of outbreaks in several countries during the 19th century. The most deaths in the last high-mortality pandemic, the 1918-19 Spanish flu, are thought to be due to bacterial secondary infections. We now have antibiotics and knowledge of clean water that will prevent a recurrence.
Cost of Pandemic Preparedness
The WHO Director General (Tedros Adhanom Ghebreyesus, February 18 at Munich Conference) stated that $31B/year is warranted for pandemic preparedness (to be ready for the ‘next one’). Bill Gates Jr. has talked about $3B/year for a ‘WHO-like body’ to coordinate. In context, the Global Fund spends less than $4B/year on malaria, tuberculosis, and HIV/AIDS combined. The annual WHO budget is roughly $3B.
In global health terms, this is a staggering amount of money. Tuberculosis (TB) kills ~1.6M every year, at a far younger mean age than Covid-19. Malaria kills nearly 400,000/year, mostly young children. Spending on each of these globally is in the $3B/year range. Converting recorded mortality to normal disease burden metrics – disability-adjusted life years (DALYs), each of these has roughly a 10 times greater burden annually in sub-Saharan Africa.
- Covax – The WHO’s Mechanism for COVID-19 Mass Vaccination
- Disease Burden in Sub-Saharan Africa
- Essential Questions to WHO on Pandemic Preparedness and Response
Debate and Discuss
Essential questions
to WHO on pandemic preparedness and response
In line with the founding principles of the WHO and orthodox principles of public health, PANDA has decided to publish its submission for the INB hearings in advance, to encourage open debate in ensuring global pandemic preparedness is underpinned by a strong evidence base, which gives full consideration to the COVID-19 response.


The Pandemic Preparedness Fallacy
COVAX - The WHO's Mechanism for COIVD-19 Mass Vaccination
This is the vehicle for supporting lower- and middle-income country Covid-19 vaccination, and therefore a good predictor of future programmes. COVAX has thus far absorbed over $7.5B, with estimates from $35.5B globally needed for 2 doses globally (Yale), to $10B for Africa (Africa CDC). The WHO is leading this push, although:
- 50% of the population of sub-Saharan Africa is below 19 yo (i.e. very young population with minimal risk).
- Nearly all now have post-infection immunity (i.e. No measurable benefit possible)
- Vaccine efficacy will wane by 6+ months, becoming negative in some studies.
There is therefore no credible benefit to African populations overall, even allowing for benefit in older, vulnerable people. Resource diversion will exacerbate the currently deteriorating population health status due to malaria, TB, HIV, and malnutrition.
This is an unsound programme, without credible public health justification. Taxpayers in the West already contributed $billions (e.g. UK. USA). It is a massive concentration of wealth sold as ‘equity’ and aid, making it emotionally difficult to oppose. Health equity is important. Vaccine equity, however, is a pharma construct that ignores the heterogeneity of health needs of populations.
We now have a whole industry built around these fallacies. Cepi, the Coalition for Epidemic Preparedness Innovation, co-founded by the Bill and Melinda Gates Foundation, is focussed predominantly on development of vaccines for pandemics. The Gavi Alliance addresses vaccines in general, but also increasingly pandemic-related interventions. These are funded by:
- Taxpayers
- Tax-free investment by specific Pharma investors (especially Bill Gates Jr. through the Bill and Melinda Gates Foundation)
- Pharma contributions.
This funding drives vaccine-related profits in Pharma, and could drive the introduction of vaccine passports (digital ID) which will also benefit some WHO sponsors.
This vehicle is clever, as it appears as aid, as well as an insurance against an imminent threat, consequently, it is easy to sell and difficult or dangerous to oppose from a public health career (or mainstream media) perspective.
Pull the wrapping off the pandemic preparedness narrative and there is little there except absorption of money by a very concentrated group of beneficiaries. The Western media is, at best, missing this, while the recent WHO treaty interest in groups skeptical of the Covid-19 response is essentially addressing a symptom, not the disease. This has been growing (arguably with considerable deliberation behind it) for the last 20 years. We believe it can be stopped only by developing a strong public understanding of the underlying facts, and the financial incentives involved. The public health institutions involved are heavily inflicted with conflict of interest, being funded by organizations driving the narrative, and will not act without such pressure.
The Pandemic Preparedness Fallacy: Statistics
Disease Burdens
in Sub-Saharan Africa
Relative estimated burdens of priority infectious diseases in sub-Saharan Africa over a 12 month period, based on reported mortality adjusted for estimated age of attack.
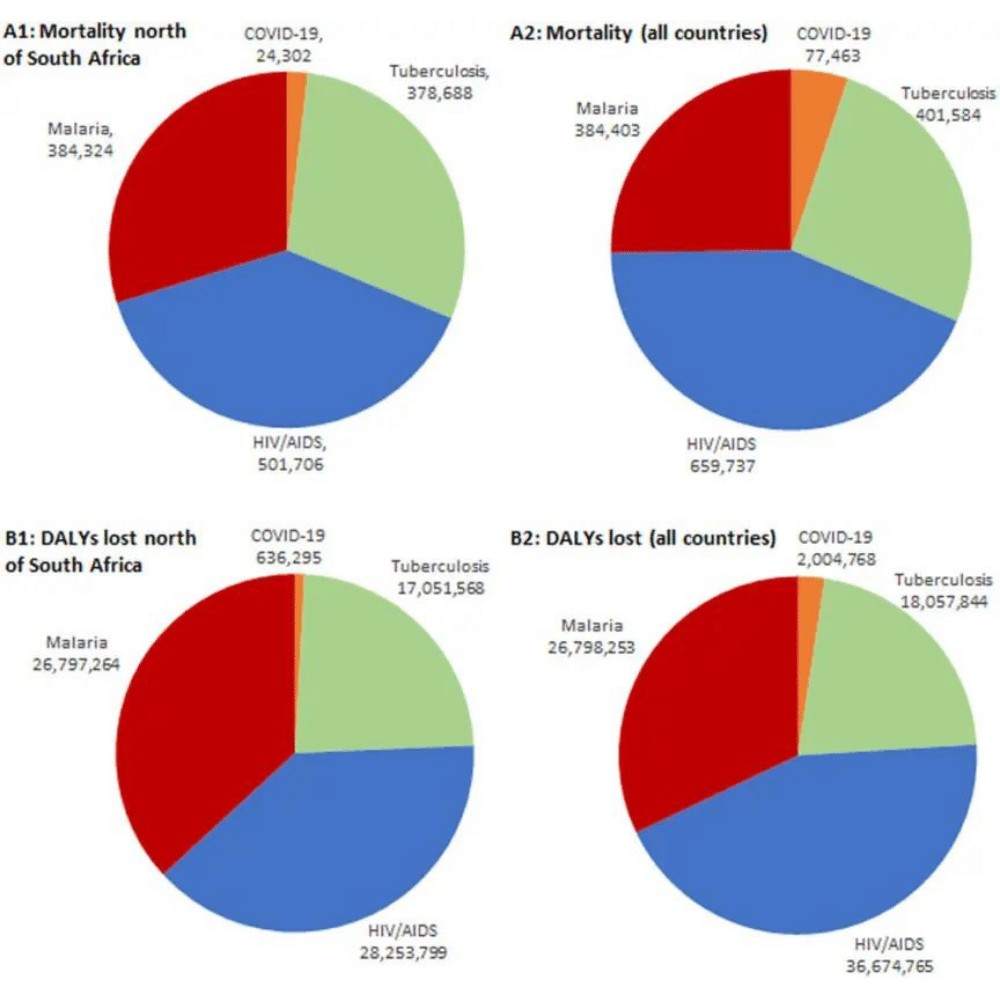
Comparison of baseline mortality and disease burdens (disability-adjusted life-years [DALYs] lost) predicted for the 12 months of 2020 for malaria, tuberculosis, and HIV/AIDS (impact before lockdown) and until March 31, 2021, for COVID-19 in sub-Saharan Africa. (A1) Mortality for sub-Saharan countries north of South Africa and Lesotho. (A2) Mortality for all sub-Saharan countries. (B1) DALYs lost for sub-Saharan countries north of South Africa and Lesotho. (B2) DALYs lost for all sub-Saharan countries.
Source: Relative Burdens of the COVID-19, Malaria, Tuberculosis, and HIV/AIDS Epidemics in Sub-Saharan Africa by David Bell and Kristian Schultz Hansen (2021

Mortality predicted for the 12 months of 2020 for malaria, tuberculosis, and HIV/AIDs (impact before lockdown) and until March 31, 2021, for COVID-19 in sub-Saharan Africa. (A) Mortality for sub-Saharan countries north of South Africa and Lesotho. (B) Mortality for all sub-Saharan countries.
Source: Relative Burdens of the COVID-19, Malaria, Tuberculosis, and HIV/AIDS Epidemics in Sub-Saharan Africa by David Bell and Kristian Schultz Hansen (2021)
Get the Background
The WHO
Pandemic Treaty
The proposed International Treaty on Pandemic Prevention and Preparedness builds on the growing reach of the International Health Regulations, in transferring more power to the World Health Organization (WHO) to declare emergencies and then require countries, under treaty obligations, to follow WHO instructions.

The WHO is a branch of the United Nations, set up in the late 1940s to support countries in managing various aspects of health. It was intended to be subject to control by member states, taking its instructions from the World Health Assembly which is made up of health ministers of member states. However, although it was originally funded by member states, it has become increasingly dependent on funding from private foundations, and corporations, particularly those heavily involved in, or invested in, the pharmaceutical industry.
In parallel with the increase in private funding, the WHO’s focus has shifted increasingly from community-based interventions to pharmaceutical-based interventions. Sister-organisations tied closely to the WHO, including the Gavi Alliance and Cepi, are also concentrated almost solely on pharmaceutical approaches. Like the WHO, they are also partly funded by tax-payers through aid budgets but heavily influenced by Pharma.
WHO staff are recruited according to national quotas, technical qualification but also personal networks. The Director-General is appointed by the vote of the health ministers, subject to international lobbying, every 4 years. As WHO staff receive relatively high rates of pay and benefits for the health sector, many spend the bulk of their career in the organization and so gain minimal external experience.
While the WHO itself has noted that pandemics are rare, recognising only 4 in the 120 years before 2020, Cepi is devoted entirely to pandemics. Funding within the WHO has also shifted increasingly toward a pandemic focus, with an emphasis on pharmaceutical (vaccine) approaches. A permanent international industry has been developed, at considerable cost, to deal with a rare problem that now depends on the declaration of new ‘pandemics’ to justify its existence.
In the context of Covid-19, it is clear that vaccine-based interventions are having a limited impact on overall outcomes, while other unprecedented interventions promoted by the WHO, against their own former pandemic guidance, have had major negative impacts on all aspects of society, including economies (massively increasing poverty), healthcare and education.
This proposed treaty raises a number of fundamental concerns that we believe should lead to its immediate abandonment:
- Countries (people) will lose sovereignty over major aspects of daily life to unelected international bureaucrats, who are subject to significant conflicts of interest from private individuals and industry.
- These WHO bureaucrats will decide on the criteria for and timing of such take-overs.
- The track record of the WHO in managing international outbreaks is poor. It is inherently dangerous to delegate control over complex issues that heavily impact the economy, society and public health to individuals in a distant location with no community or relevant national affiliations, and no direct stake in the outcomes.
- Such centralization is contrary to the fundamental pillars of community-based, locally organised healthcare, and antithetical to the principles of individual rights and autonomy upon which the WHO’s constitution is based.
- The increasing emphasis on pandemics instead of on the actual major causes of human illness and mortality is inappropriate, and the diversion of funds and activity will have hugely negative impacts on overall population and individual health.
The world needs international forums for sharing data, for concentrating technical expertise to support countries lacking these and to facilitate discussions between countries concerning health issues, including emergencies. Such organisations must be in service of member countries and their people, not act as unelected authorities, funded and influenced by conflicted, non-national interests that attempt to direct and control the lives of free citizens.
This proposed treaty raises a number of fundamental concerns that we believe should lead to its immediate abandonment:
Countries (people) will lose sovereignty over major aspects of daily life to unelected international bureaucrats, who are subject to significant conflicts of interest from private individuals and industry.
These WHO bureaucrats will decide on the criteria for and timing of such take-overs.
The track record of the WHO in managing international outbreaks is poor. It is inherently dangerous to delegate control over complex issues that heavily impact the economy, society and public health to individuals in a distant location with no community or relevant national affiliations, and no direct stake in the outcomes.
Such centralization is contrary to the fundamental pillars of community-based, locally organised healthcare, and antithetical to the principles of individual rights and autonomy upon which the WHO’s constitution is based.
The increasing emphasis on pandemics instead of on the actual major causes of human illness and mortality is inappropriate, and the diversion of funds and activity will have hugely negative impacts on overall population and individual health.
The world needs international forums for sharing data, for concentrating technical expertise to support countries lacking these and to facilitate discussions between countries concerning health issues, including emergencies. Such organisations must be in service of member countries and their people, not act as unelected authorities, funded and influenced by conflicted, non-national interests that attempt to direct and control the lives of free citizens.

Get The Background
The International
Health Regulations
The IHR amendments, proposed by the United States, build on the existing IHR that were introduced in 2005 and are binding under international law. While many are unaware of this mechanism, it already enables a WHO DG to declare public health emergencies of international concern and recommend measures be taken such as border closures to isolate countries and restrict the movement of people.
The draft document includes proposals to:
Establish an ‘emergency committee’ to assess health threats and outbreaks and recommend responses.
Establish a ‘country review mechanism’ to assess compliance of countries with the various WHO recommendations / requirements regarding pandemic preparedness, which include surveillance and reporting measures. This appears to be modelled on the UN’s human rights country review mechanism. Where their internal programs are considered inadequate, countries would then be issued with requirements to bring them into compliance, on the request of another State party (country).
Expand the scope for the WHO DG and Regional Directors to declare public health emergencies and instruct border closures, interruption and removal of rights to travel and potentially internal ‘lockdown’ requirements. This will remove the necessity of local country consultation, and expand the power to send teams of WHO personnel to countries to investigate outbreaks, irrespective of the findings of the emergency committee.
Reduce the usual review period for countries to internally discuss and opt out of such mechanisms to just 6 months (rather than 18 months for the original IHR), and then implement them after a 6-month notice period.
Regional Directors, of which there are 6, will be empowered to declare regional ‘public health emergencies’, irrespective of a decision by the DG.
These amendments will be discussed and voted on at the World Health Assembly on 22-28 May 2022 and may require only a simple majority of countries present to come into law, consistent with Article 60 of the WHO constitution. For clarity, this means countries such as Nuie, with 1300 people, have an equal weight on the voting floor to India, with 1.3 billion people. Countries must then signal their intent to opt out of the new amendments within 6 months.
These measures will become legally binding as articles of the IHR. Therefore heavy pressure will be applied to governments to comply with the dictates of the WHO DG and the unelected bureaucrats that comprise the organisation, and thus also the external actors who are influential in WHO decision-making processes.
Discover More
Related Articles & Papers
magine control of all future responses to virus outbreaks – influenza, for instance – being dictated to the entire world by a cadre of unelected health bureaucrats in a distant country or continent.
Since 2000, the WHO has become increasingly dependent on private foundations and pharmaceutical companies for funding. As their influence has grown, the balance of power has shifted away from populations. This move has moved them away from a global institution which aims to provide access to good health for all, regardless of socioeconomic status.
The mechanisms for increasing direct WHO control of pandemics through the International Health Regulations and the WHO Pandemic Treaty have strong backing from private sector funders of the WHO and from many national governments. And the most likely scenario for preventing the adoption of the two new mechanisms is for populations in democratic States to stimulate open debate.
magine control of all future responses to virus outbreaks – influenza, for instance – being dictated to the entire world by a cadre of unelected health bureaucrats in a distant country or continent.
Since 2000, the WHO has become increasingly dependent on private foundations and pharmaceutical companies for funding. As their influence has grown, the balance of power has shifted away from populations. This move has moved them away from a global institution which aims to provide access to good health for all, regardless of socioeconomic status.
The mechanisms for increasing direct WHO control of pandemics through the International Health Regulations and the WHO Pandemic Treaty have strong backing from private sector funders of the WHO and from many national governments. And the most likely scenario for preventing the adoption of the two new mechanisms is for populations in democratic States to stimulate open debate.
Take Action
The Proposed WHO Pandemic "Treaty" is a Major Threat
to Global Health and Human Rights
The Proposed WHO Pandemic "Treaty" is a Major Threat to Global Health and Human Rights
Raise your objections to the proposed pandemic treaty by sending this letter to your MP or government representative.
The pandemic ‘treaty’ proposed by the WHO is a symptom, not a cause, of this major diversion of global health resources from community-based and high-burden endemic disease programmes, to the purchase and mandating of pharmaceuticals for relatively rare outbreaks with far lower mortality. PANDA believes this is a major threat to human rights and to global health.
PANDA will be highlighting the processes that have led to this situation and potential harms, defining alternative approaches that promise greater benefit to society and health, and initiating and supporting efforts to advocate for, and realise, such approaches.


Lead Author
David Bell
PHD Public Health
David is a clinical and public health physician with a PhD in population health and background in internal medicine, modelling and epidemiology of infectious disease. Previously, he was Director of the Global Health Technologies at Intellectual Ventures Global Good Fund in the USA, Programme Head for Malaria and Acute Febrile Disease at FIND in Geneva, and coordinating malaria diagnostics strategy with the World Health Organization. David maintains that accurate data and balanced evidence is available to the public, and other decision-makers, in order to make decisions that are in everyone’s best interests. David Bell is an executive board member of PANDA.